Menopause is a natural stage in the life of every woman and is characterized by a gradual and consistent fading of her reproductive functions. However, according to the results of multicenter studies, up to 60% of women suffer from manifestations of the menopausal syndrome, which can significantly reduce the quality of life, labor potential and negatively affect social and creative activity [1, p. 875].
Significant clinical manifestations and consequences of the menopausal syndrome include vasomotor symptoms (hot flashes, increased sweating, headaches, blood pressure changes, palpitations, tinnitus, dizziness), psychoemotional symptoms (weakness, frequent feelings of anxiety and restlessness, memory loss, decreased concentration, insomnia), urogenital symptoms (vaginal dryness, dyspareunia, dysuria), sexual disorders (decreased libido), symptoms of the musculoskeletal system (joint and muscular pain), metabolic disorders (osteoporosis, atherosclerosis, cardiovascular diseases) [2, p. 752].
Recommendations of modern unified clinical protocols of primary, secondary (specialized), tertiary (highly specialized) medical care regulate a personalized approach to the correction of menopausal disorders and provide for the application of both non-drug and drug (non-hormonal, hormonal) treatment methods [3, p. 72]. It should be emphasized that menopausal hormone therapy (MHT) is currently recognized as the most effective, which is due to its undoubted clinical and pathogenetic focus and the widespread use of innovative technologies in modern pharmacology [4, p. 25]. However, MHT has a number of absolute and relative contraindications for use as well as it can be accompanied by certain complications and side effects that the doctor must take into account in his practice. Therefore, according to the requirements, before starting MHT, the doctor must carry out a number of measures aimed at identifying and analyzing concomitant diseases of the internal organs in the patient, risk factors for cardiovascular and oncological pathology [5, p. 6].
The aim of our study was to determine the overall cardiovascular risk in patients with the menopausal syndrome who were prescribed MHT.
This clinical study involved 128 women aged 45-60 years who suffered from menopausal syndrome manifestations.
During the study, a general and obstetric-gynecological anamnesis, results of the objective examination and instrumental-laboratory tests were analyzed according to modern clinical guidelines. To determine the severity of the menopause symptoms, the Menopause Rating Scale was used [6, p. 2]. To determine the cardiovascular risk, the SCORE (Systemic Coronary Risk Estimation) scale was used, which included several assessed parameters: systolic blood pressure, smoking (yes/no), total cholesterol in blood plasma (mmol/l), age and sex of the patient [7, p. 3].
The study results were processed using methods accepted in medical and biological research. The material was processed using methods of variation and correlation analysis using standard and specialized computer programs.
Among the examined patients, normal BP indices (120-129 and/or 80-84 mm Hg) were noted in 33 (25.8%) women, high normal BP (130-139 and/or 85-89 mm Hg) - in 54 (42.2%), arterial hypertension was diagnosed in 41 (32.0%). At the same time, stage I hypertension (uncomplicated) was diagnosed in 26 (63.4%), stage II (asymptomatic disease) - 11 (26.8%), stage III (established disease) - in 4 (9.8%). The grade I hypertension (BP 140-159 and/or 90-99 mmHg) was noted in 34 (82.9%) women suffering from manifestations of the menopausal syndrome, grade II (BP 160-179 and/or 100-109 mmHg) – in 7 (17.1%).
18 (14.1%) women answered positively to the question about smoking cigarettes containing tobacco.
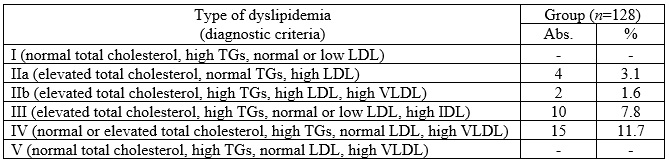
The next step of our study was the analysis of lipidogram of the patients in the examined group (Table 1). The levels of triglycerides (TGs), total cholesterol, low-density lipoproteins (LDL), very-low-density lipoproteins (VLDL), intermediate-density lipoproteins (IDL) were assessed in order to determine the type of dyslipidemia (I, IIa, IIb, III, IV, V) according to Friedrickson Lipoprotein Patterns [8, p. 2].
Thus, among the patients suffering from manifestations of the climacteric syndrome, 31 (24.2%) had lipid metabolism disorders. Dyslipidemia type IIa was diagnosed in 4 (3.1%), IIb - in 2 (1.6%), III - in 10 (7.8%), IV - in 15 (11.7%) women. It should be noted that IIa, IIb, III types of dyslipidemia have a high risk of atherogenic damage to peripheral arteries and cardiovascular diseases, type IV is characterized by moderate atherogenicity.
Table 1
Dyslipidemia in patients suffering from the menopausal syndrome
The final step of our study was to determine the cardiovascular risk category (low (<1%), moderate (≥1 and <5%), high (≥5 and <10%), and very high (≥10%)) using the SCORE scale. Among the patients suffering from climacteric syndrome, 104 (81.3%) women had a low risk of developing fatal cardiovascular diseases over the next 10 years, with 15 (11.7%) having a moderate risk and 9 (7.0%) having a high risk. Thus, in 11.7% of the patients with manifestations of climacteric syndrome, the prescription of MHT should be clearly reasoned and balanced, and in 7.0% it is contraindicated.
Conclusions:
1. Approximately every fifth woman suffering from the climacteric syndrome has an increased individual risk of developing atherosclerotic cardiovascular diseases;
2. Determination of the cardiovascular risk is of great multidisciplinary significance, which allows the physician to assess the appropriateness and safety of MHT, and in case of its increase, promptly refer the patient for additional examination to select a system of necessary preventive and therapeutic measures.
References:
1. Nappi RE, Kroll R, Siddiqui E, Stoykova B, Rea C, Gemmen E, Schultz NM. Global cross-sectional survey of women with vasomotor symptoms associated with menopause: prevalence and quality of life burden. Menopause. 2021 May 24;28(8):875-882. doi: 10.1097/GME.0000000000001793. Erratum in: Menopause. 2022 Jun 01;29(6):759. doi: 10.1097/GME.0000000000001996. PMID: 34033602; PMCID: PMC8746897.
2. Choi HR, Chang Y, Kim Y, Cho Y, Kwon MJ, Kang J, Kwon R, Lim GY, Kim KH, Kim H, Hong YS, Park J, Zhao D, Cho J, Guallar E, Park HY, Ryu S. Vasomotor and other menopause symptoms and the prevalence of ideal cardiovascular health metrics among premenopausal stage women. Menopause. 2023 Jul 1;30(7):750-757. doi: 10.1097/GME.0000000000002203. PMID: 37279516; PMCID: PMC10309111.
3. Meeta M, Digumarti L, Agarwal N, Vaze N, Shah R, Malik S. Clinical Practice Guidelines on Menopause: *An Executive Summary and Recommendations: Indian Menopause Society 2019-2020. J Midlife Health. 2020 Apr-Jun;11(2):55-95. doi: 10.4103/jmh.JMH_137_20. Epub 2020 Aug 10. PMID: 33281418; PMCID: PMC7688016.
4. Chaikittisilpa S, Orprayoon N, Vallibhakara O, Vallibhakara SA, Tanmahasamut P, Somboonporn W, Rattanachaiyanont M, Techatraisak K, Jaisamrarn U. Summary of the 2023 Thai Menopause Society Clinical Practice Guideline on Menopausal Hormone Therapy. J Menopausal Med. 2024 Apr;30(1):24-36. doi: 10.6118/jmm.24006. PMID: 38714491; PMCID: PMC11103073.
5. Cho L, Kaunitz AM, Faubion SS, Hayes SN, Lau ES, Pristera N, Scott N, Shifren JL, Shufelt CL, Stuenkel CA, Lindley KJ; ACC CVD in Women Committee. Rethinking Menopausal Hormone Therapy: For Whom, What, When, and How Long? Circulation. 2023 Feb 14;147(7):597-610. doi: 10.1161/CIRCULATIONAHA.122.061559. Epub 2023 Feb 13. PMID: 36780393; PMCID: PMC10708894.
6. Heinemann LA, Potthoff P, Schneider HP. International versions of the Menopause Rating Scale (MRS). Health Qual Life Outcomes. 2003 Jul 30;1:28. doi: 10.1186/1477-7525-1-28. PMID: 12914663; PMCID: PMC183844.
7. Csenteri O, Jancsó Z, Szöllösi GJ, Andréka P, Vajer P. Differences of cardiovascular risk assessment in clinical practice using SCORE and SCORE2. Open Heart. 2022 Nov;9(2):e002087. doi: 10.1136/openhrt-2022-002087. PMID: 36442905; PMCID: PMC9710472.
8. Sampson M, Ballout RA, Soffer D, Wolska A, Wilson S, Meeusen J, Donato LJ, Fatica E, Otvos JD, Brinton EA, Rosenson RS, Wilson P, Amar M, Shamburek R, Karathanasis SK, Remaley AT. A new phenotypic classification system for dyslipidemias based on the standard lipid panel. Lipids Health Dis. 2021 Nov 27;20(1):170. doi: 10.1186/s12944-021-01585-8. PMID: 34838008; PMCID: PMC8627634.
|